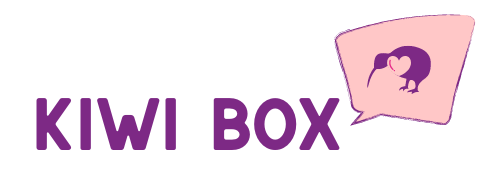
When someone starts to show signs of memory loss, confusion, or difficulty with language, it’s common to hear people use the terms Alzheimer’s and dementia interchangeably. But while they’re closely related, they’re not the same thing. Understanding the difference can be the key to getting an accurate diagnosis, choosing the right treatments, and supporting your loved one with clarity and confidence.
In this article, we’ll break down what dementia really is, how Alzheimer’s fits into that picture, and why these distinctions matter – especially when it comes to planning care and setting expectations.
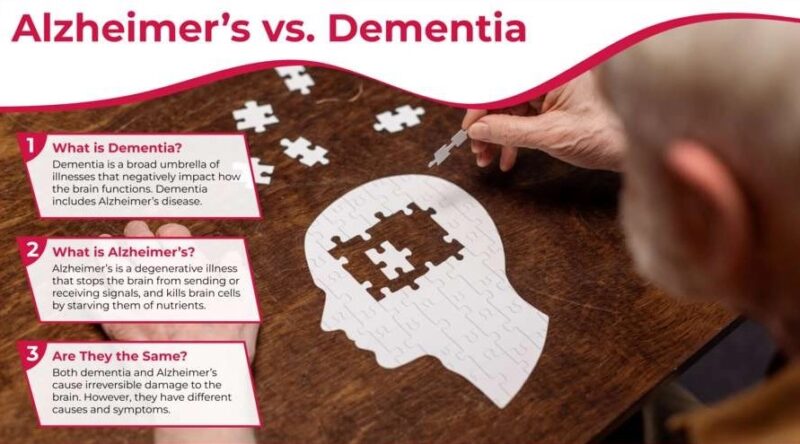
Alzheimer’s vs. Dementia: Comparison table
| Feature | Dementia | Alzheimer’s Disease |
| What it is | General term for a group of symptoms affecting memory and thinking | A specific, progressive brain disease that causes dementia |
| Cause | Can be caused by Alzheimer’s, strokes, Parkinson’s, infections, and more | Caused by abnormal protein buildup (plaques and tangles) in the brain |
| Is it a diagnosis? | No – it’s a syndrome, not a disease | Yes – it’s a clinical diagnosis |
| Common symptoms | Memory loss, confusion, language problems, impaired judgment | Memory loss (especially recent), disorientation, trouble with familiar tasks |
| Onset of symptoms | Varies depending on type and cause | Gradual, often starting with short-term memory loss |
| Progression | May be reversible (in rare cases), stable, or progressive | Always progressive – symptoms worsen over time |
| Treatment options | Depends on the underlying cause | Medications can help manage symptoms but no cure |
| Most common type | Alzheimer’s accounts for 60–80% of dementia cases | Alzheimer’s is the most common type of dementia |
| Other types included | Vascular, Lewy body, frontotemporal, mixed dementia | Not applicable |
| Prognosis | Varies greatly by cause | Predictable decline through alzheimers stages |
What is dementia?

Dementia is not a specific disease – it’s an umbrella term used to describe a set of symptoms that affect memory, reasoning, communication, and the ability to perform daily tasks. It’s caused by damage to brain cells, which interferes with their ability to communicate with each other.
People with dementia may experience:
- Difficulty remembering recent events
- Trouble with language or finding words
- Poor judgment and decision-making
- Changes in mood or personality
- Disorientation, even in familiar places
Think of dementia the same way you would think of “fever” – it’s a general indicator that something is wrong, but it doesn’t tell you the cause. That’s where specific diagnoses, like Alzheimer’s disease, come in.
What is Alzheimer’s disease?
Alzheimer’s disease is the most common cause of dementia, accounting for 60–80% of all dementia cases. It is a specific, progressive brain disease marked by the buildup of abnormal proteins (amyloid plaques and tau tangles) that damage brain cells over time.
What sets Alzheimer’s apart is the pattern and progression of its symptoms. It typically begins with short-term memory loss and gradually advances into more severe cognitive decline, affecting speech, mobility, and behavior.
Some defining features of Alzheimer’s:
- Gradual, predictable progression
- Memory loss is typically the first and most obvious symptom
- Changes in the brain can begin 10–20 years before symptoms appear
- No current cure, though treatments can help manage symptoms
For a clearer understanding of the symptomatic progression, alzheimers stages are categorized into early, middle, and late stages, each with distinct challenges and care needs.
The progression of Alzheimer’s varies from person to person, influenced by genetic factors, overall health, and environmental conditions. Proactive monitoring of symptoms and the related progression is vital to managing the disease.
Medical interventions and care strategies must be adapted to the individuals’ evolving needs, emphasizing the importance of a personalized approach to treatment and support.
How are Alzheimer’s and dementia diagnosed?
Diagnosis begins with a comprehensive evaluation, which may include:
- A medical history review
- Cognitive tests (e.g., memory, reasoning, language)
- Brain imaging (MRI or CT scans)
- Blood work and neurological exams
Doctors aim to rule out reversible causes of dementia-like symptoms first – including vitamin deficiencies, medication interactions, thyroid issues, or infections.
Once other causes are excluded, and a clear pattern of progression emerges, specialists may diagnose a type of dementia, such as Alzheimer’s, vascular dementia, Lewy body dementia, or frontotemporal dementia.
Other types of dementia besides Alzheimer’s
Understanding the difference between Alzheimer’s and dementia also means knowing there are multiple types of dementia, each with its own characteristics:
| Type of Dementia | Key Features |
| Vascular dementia | Often follows a stroke; caused by reduced blood flow to the brain |
| Lewy body dementia | Visual hallucinations, Parkinson-like movement symptoms |
| Frontotemporal dementia | Affects behavior and language first rather than memory |
| Mixed dementia | Combination of two or more types (often Alzheimer’s and vascular) |
Each form affects the brain differently and may require tailored treatment strategies.
Why the distinction matters for care
Knowing the difference between Alzheimer’s and other types of dementia is critical for several reasons:
- Treatment and medications:
Some drugs approved for Alzheimer’s (like donepezil or memantine) may not be helpful – or may even be harmful – for other types of dementia. - Progression planning:
Alzheimer’s has a relatively predictable trajectory. Other dementias can progress more suddenly or have different symptoms entirely. - Family education and expectations:
Families can better support loved ones when they understand the specific symptoms they’re likely to face. - Legal and financial planning:
Knowing the expected timeline helps with decisions around long-term care, power of attorney, and living arrangements.
Common misconceptions
Because these terms are so often misunderstood, let’s clear up a few frequent myths:
- Myth: Dementia is a normal part of aging
Fact: While memory does decline with age, dementia is not inevitable. - Myth: Alzheimer’s is the only kind of dementia
Fact: Alzheimer’s is just the most common type. - Myth: You can’t live well with dementia
Fact: With support, many people live meaningful lives for years after diagnosis.
When to seek help
If you or a loved one are experiencing memory problems or cognitive changes that interfere with daily life, don’t wait to speak with a doctor. Early detection allows for:
- Access to treatments that may slow progression
- Time to make informed decisions about care and lifestyle
- Emotional preparation for what’s ahead
The earlier you know what you’re dealing with – whether it’s Alzheimer’s or another form of dementia – the better equipped you’ll be.
Final thoughts
It’s easy to confuse dementia and Alzheimer’s – especially when you’re hearing both terms tossed around during a difficult time. But getting clear on the distinction empowers you to ask better questions, pursue the right treatments, and support your loved one with understanding, not guesswork.
Knowing what you’re dealing with is the first step toward managing it. And while no form of dementia is easy, education, preparation, and compassion make all the difference.