When it comes to enhancing cognitive performance, managing neuropsychiatric symptoms, or optimizing brain health, the choice of intervention is not trivial.
Patients, clinicians, and wellness practitioners now have access to a wide array of brain training modalities – from neurofeedback and cognitive behavioral-based programs to computerized cognitive training and transcranial direct current stimulation (tDCS).
The critical question is: Which approach aligns best with your neurological profile, therapeutic goals, and evidence-based safety parameters?
Comparison of Brain Training Methods
| Method | Primary Mechanism | Typical Applications | Evidence Strength | Session Frequency | Safety Profile |
|---|---|---|---|---|---|
| Neurofeedback | EEG/fMRI-based real-time modulation of brainwave patterns | ADHD, anxiety, insomnia, epilepsy, post-concussion syndrome | Moderate to strong (condition-specific) | 20–40 sessions | Non-invasive, minimal adverse effects |
| Computerized Cognitive Training | Software-driven tasks improving working memory, attention, and processing speed | Age-related cognitive decline, post-stroke rehabilitation | Moderate | 3–5 sessions/week | Very safe, screen-related eye strain possible |
| Cognitive Behavioral Therapy (CBT)-based Brain Training | Psychological interventions rewiring maladaptive thought patterns | Anxiety disorders, depression, OCD | Strong | Weekly over several months | Safe, dependent on therapist skill |
| tDCS (Transcranial Direct Current Stimulation) | Low electrical current modulating cortical excitability | Depression, chronic pain, cognitive enhancement | Moderate | Daily to weekly | Generally safe; mild tingling, headaches |
| Brainwave Entrainment (Binaural Beats) | Auditory/visual stimuli inducing specific frequency states | Relaxation, focus, sleep optimization | Weak to moderate | As desired | Safe for most, avoid in epilepsy |
Mechanisms, Clinical Protocols, and Regulatory Considerations in Neurofeedback
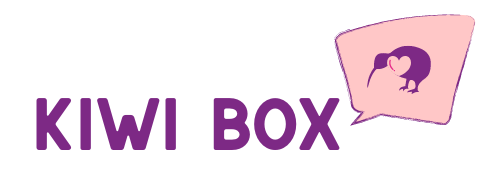
Neurofeedback, also known as EEG biofeedback, is a closed-loop neuromodulation system designed to train self-regulation of cortical activity. Using surface electrodes, a quantitative electroencephalogram (qEEG) is recorded in real time.
These data are processed and presented to the patient via visual or auditory cues, creating a feedback loop that enables conscious modulation of brainwave patterns. The aim is to induce long-term neuroplastic adaptations, allowing the central nervous system to sustain optimal arousal and cognitive states without ongoing external intervention.
Clinical protocols are highly individualized. Baseline qEEG mapping identifies deviations from normative brainwave distributions, guiding targeted interventions in specific frequency bands:
- Beta (13–30 Hz) – linked to concentration and task engagement.
- Alpha (8–12 Hz) – associated with relaxed wakefulness.
- Sensorimotor rhythm (SMR, 12–15 Hz) – implicated in motor control and stability.
A frequent question in clinical settings is whether neurofeedback FDA approved for therapeutic use. The FDA has cleared certain neurofeedback devices for relaxation training, but broader clinical claims remain under “adjunctive” status pending high-quality randomized controlled trials (RCTs).
Current evidence supports its application in ADHD, anxiety, epilepsy, and post-concussive symptoms, but practitioners must operate within regulatory frameworks and informed consent protocols.
Adaptive Algorithm-Based Cognitive Enhancement in Computerized Cognitive Training (CCT)

Computerized Cognitive Training (CCT) encompasses software-mediated interventions designed to enhance targeted cognitive domains, including working memory, processing speed, selective attention, and executive control.
Unlike neurofeedback, CCT does not monitor brainwave activity; instead, it employs performance-dependent adaptive algorithms that dynamically adjust difficulty based on the user’s responses, promoting incremental skill acquisition.
CCT is frequently deployed in:
- Post-stroke neurorehabilitation, to restore executive function and visuospatial skills.
- Mild Cognitive Impairment (MCI), as a preventative measure against dementia progression.
- Aging populations, to mitigate age-related decline in processing efficiency.
Meta-analytic data suggest moderate improvements in targeted domains, but transfer effects – the generalization of gains to untrained abilities or real-world activities – are inconsistent. Efficacy depends on intensity (typically 3–5 weekly sessions over several months) and user engagement.
Unlike tDCS or neurofeedback, CCT carries no bioelectrical modulation risk, making it particularly suitable for populations where neuromodulation is contraindicated (e.g., individuals with seizure disorders or implanted medical devices). However, clinicians should manage expectations, emphasizing that CCT is best employed as part of a multimodal cognitive health program.
Psychotherapeutic Neuroplasticity Through Cognitive Behavioral Therapy-Based Brain Training

Cognitive Behavioral Therapy (CBT)-based brain training operates on the principle of behavioral neuroplasticity – the intentional restructuring of maladaptive thought patterns and behaviors to elicit favorable neuropsychological outcomes. Unlike neurofeedback, which modifies electrophysiological activity directly, CBT engages top-down cortical processes via structured therapeutic exercises.
For anxiety disorders, interventions may include graduated exposure protocols, cognitive restructuring to challenge maladaptive beliefs, and mindfulness-based attentional control.
In depression, CBT modules often emphasize behavioral activation, cognitive reframing, and problem-solving skills.
The neurobiological underpinning of CBT-based training involves strengthening functional connectivity within prefrontal-limbic circuits, thereby improving emotional regulation and cognitive flexibility.
Clinical evidence for CBT is robust, with numerous RCTs confirming its efficacy for mood and anxiety disorders, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD).
However, CBT’s therapeutic curve is gradual – typically spanning several months – and its success is heavily dependent on patient adherence and therapist proficiency.
While it lacks the rapid neurophysiological modulation of neurofeedback or tDCS, its effects are durable and often persist after therapy concludes, making it an evidence-based choice for chronic conditions.
Electrophysiological Modulation in Transcranial Direct Current Stimulation (tDCS)

Transcranial Direct Current Stimulation is a non-invasive brain stimulation (NIBS) modality that applies subthreshold direct electrical currents (typically 1–2 mA) through scalp electrodes to modulate cortical excitability. The polarity of stimulation determines the neuromodulatory effect:
- Anodal stimulation depolarizes neuronal membranes, increasing the likelihood of action potential firing.
- Cathodal stimulation hyperpolarizes membranes, inhibiting cortical activity in the targeted area.
tDCS has been studied extensively in major depressive disorder, neuropathic pain, stroke recovery, and cognitive enhancement in healthy adults. While effects are often subtle compared to invasive neuromodulation (e.g., deep brain stimulation), repeated tDCS sessions can yield measurable improvements in targeted domains.
Administration requires precise electrode placement based on neuroanatomical targeting (e.g., dorsolateral prefrontal cortex for depression, motor cortex for motor recovery). Incorrect electrode configuration or excessive stimulation duration may reduce efficacy or induce mild adverse effects such as transient headaches, tingling, or skin irritation.
tDCS is generally well tolerated, but professional oversight is essential, especially when integrated into a broader neurorehabilitation program involving pharmacological or behavioral interventions.
Neural Oscillation Modulation Through Brainwave Entrainment and Related Adjunctive Therapies

Brainwave entrainment techniques seek to influence endogenous neural oscillations via rhythmic sensory stimuli. Common modalities include:
- Binaural beats – two tones of slightly different frequencies presented separately to each ear, producing a perceived third tone corresponding to the frequency difference.
- Photic stimulation – rhythmic light flashes designed to induce neural synchrony.
The intended outcome is to shift brainwave dominance toward desired frequency ranges, such as alpha (relaxation), theta (meditative states), or beta (alertness). While EEG studies have documented short-term changes in frequency power following entrainment, long-term neuroplastic effects remain insufficiently validated.
These methods are generally positioned as adjunctive wellness interventions rather than primary clinical treatments. They are often marketed for relaxation, focus enhancement, or sleep improvement. While safe for most users, they are contraindicated in individuals with photosensitive epilepsy due to the risk of seizure induction.
In clinical practice, brainwave entrainment may serve as a low-cost, accessible supplement to more evidence-backed therapies such as neurofeedback or CBT, but should not replace them when treating diagnosable neurological or psychiatric conditions.
Factors to Consider Before Choosing a Method
Selecting the right brain training approach involves evaluating multiple parameters:
- Clinical Indication – Neurological vs. psychiatric vs. cognitive wellness goals.
- Evidence Quality – Peer-reviewed clinical trials supporting the specific application.
- Duration and Commitment – Number of sessions, time per session, and adherence requirements.
- Safety and Contraindications – Presence of seizure disorders, implanted devices, or psychiatric instability.
- Cost and Accessibility – Availability of trained practitioners, equipment, and follow-up options.
When to Seek Professional Guidance and Assessment
Choosing an appropriate brain training method is safest under the direction of a neurologist, neuropsychologist, or rehabilitation specialist. These professionals can perform a baseline neurocognitive evaluation – including qEEG, neuropsychological testing, and in some cases, functional imaging – to align the intervention with the patient’s specific cortical activity profile.
In cases involving epilepsy, post-traumatic brain injury, or neurodegenerative diseases, clinical oversight is critical to prevent adverse effects and ensure optimal outcomes. For example, poorly matched neurofeedback protocols or incorrect tDCS electrode placement can exacerbate symptoms.
Specialists can also integrate brain training into a comprehensive treatment plan, combining pharmacologic therapy, psychotherapy, and rehabilitation strategies to maximize safety and therapeutic gains while monitoring patient progress over time.
Conclusion
No single brain training method is universally “best.”
Neurofeedback offers a direct neural feedback loop with promising applications across clinical and wellness settings, but it requires specialized equipment and trained practitioners. Cognitive training programs are accessible and safe but may yield narrower benefits. Non-invasive brain stimulation techniques like tDCS carry a different risk-benefit profile and require precise administration.
The optimal choice hinges on individual goals, medical history, and the strength of supporting evidence. A comprehensive evaluation – ideally involving neuroimaging or neurocognitive testing – can ensure that the method selected delivers both efficacy and safety.